- Москва, ул.Лётчика Грицевца 14а,
м. «Пыхтино» - Ежедневно, с 1200 до 2000
- +7 (915) 000-77-99 - (Телефон салона) +7 (915) 000−77−99 - (WhatsApp)+7 (915) 000−77−99 - (Viber)
- domtattoo@yandex.ru
Pitfalls and Recommendations in Cases of Laser Removal
Все о татуировках
- Стили татуировки
- Белая татуировка
- Биомеханика (Biomechanics) и Органика
- Блэкворк ( Blackwork)
- Дотворк (Dotwork)
- Готика «Gothic»
- Кельтские
- Клокворк
- Нью Скул ( New School)
- Олд Скул ( Old School)
- Ориентал (Oriental)
- Полинезия
- Реализм
- Стимпанк
- Сюрреализм (Сверхреализм)
- Трайбл (Tribal)
- Треш полька
- Черно-серая "Black&grey"
- Чикано (Chicano)
- Этнический стиль тату (Ethnic)
- Японские тату
- Тотемные тату Тлинкитов
- Татуировки- надписи
- Временная татуировка.
- Хоррор
- Парные тату
- Крестиком
- Кружева
- Ультрафиолетовая татуировка
- Татуировки на частях тела
- Надписи для тату с переводом
- Надписи с переводом с немецкого на русский язык
- Надписи, афоризмы, цитаты на португальском и бразильском языке с переводом на русский
- Надписи на испанском с переводом
- Перевод фраз и гимнов (стихов) с хинди на русский
- Фразы, надписи и афоризмы на арабском языке с переводом
- Надписи для мужчин
- Надписи для девушек
- Вопросы о татуировках
- Астрология и астральная геометрия
- Значение тату
- Уход за татуировкой
- Для СМИ и видео проектов
- Татуировка на шрамах
- Иглы и краски для татуировок
- Зодиакальные татуировки...
- Стили, виды татуировки. Сведение тату.
- English language
- Все о Сак Янт - Тайской Шаманской Татуировки
- Священные татуировки - ИЗ ПРОШЛОГО
- МАГИЧЕСКИЕ ЧЕРНИЛА: ЗАКЛИНАНИЯ И СИГИЛЫ
- ИГЛОЙ НА КОЖЕ
- ЛУК СИТ
- КХРУ САК
- ВИЧА
- ТЕКСТЫ И ЧИСЛА, ТЕЛЕСНЫЙ ЩИТ
- ЯНТРЫ ЧОК ЛАП ПРИНОСЯТ УДАЧУ И ПРОЦВЕТАНИЕ.
- ТРАНС
- ТРАДИЦИИ САК ЯНТ В ТАИЛАНДЕ
- ЗАКЛИНАНИЯ И ПИСЬМЕНА
- Обучение мастеров-татуировки в Тайланде (ТРАНСФОРМАЦИЯ И ДИСЦИПЛИНА)
- Сигилизм
Информация
- Портфолио
- Все о пирсинге
- Виды и стили
- Подготовка и процедура пирсинга
- Когда пирсинг уже сделан
- Бод Мод
- Украшение для пирсинга
- Инструмент для пирсинга
- Словарь терминов
- Cтоимость пирсинга
- Магическое, символическое значение пирсинга
- Вопросы и ответы про пирсинг
- Удаление татуировок
- Все о татуаже
- Новости
- Ответы на часто задаваемые вопросы о тату.
- Работы тату художника Yann Travaille
- Съемки MTV
- Проба пера
- Съемки Дискавери в судии ...
- Энциклопедия пирсинга
- 7 Московская Международная Тату Конвенция
- «Звёздный» гость салона «Дом Элит Тату» - известный продюсер Андрей Клюкин
- Ушел из жизни тату мастер Илья Смирнов
- Мы примим участие в Питерской тату конвенции 2015 года
- У нас делают татуировки модели Creepy Sweets
- Оригинальный майки и футболки с аэрографией за 4.000 рублей
- Мы получили независимую премию "Лучший Тату Салон 2015 года" по версии портала Татуировка.Рф
- Мы участники и победители тату конвенции в Москве
- Мы организаторы "Ночи Татуировщика 2015 в Москве"
- Rock heroes: Miss Тату Хабаровск
- Немецкий политик сядет в тюрьму за то что сделал нацистскую татуировку
- Международная Московская Тату Конвенция 2016
- Санкт-Петербургский Тату-Фестиваль
- 2 Международный фестиваль татуировки Сочи 2016
- Самый старый татуированный человек на нашей планете.
- 9-я Международная Московская Тату Конвенция 2017
- Тату мастер с 1.4 миллионом подписчиков маскирует растяжки
- Miss Tattoo Australia Дженн Десмонд - водитель грузовика
- Тату разрешены
- Зейн Малик сделал татуировку с глазами Джиджи Хадид на груди
- Тату как запрет на реанимацию
- В честь ЛДПР прошла тату-вечеринка
- Тату салон в Самаре
- Аренда места в тату салоне Москва. Как правильно и главное где арендава
- Обучение и все о нем
IMPORTANCE Pigmented lesions in decorative tattoos cause diagnostic difficulties at a clinical and dermoscopic level. In cases of laser removal of tattoos, hidden suspicious nevi may be revealed gradually.
OBSERVATIONS We describe the first case of a malignant melanoma that developed on a preexisting nevus within a tattoo during and between the phases of laser removal. The patient refused to undergo excision of the nevus until we made excision conditional for continued laser treatment.
CONCLUSIONS AND RELEVANCE The English literature reports 16 cases of malignant melanoma developing in tattoos. Correlation between the placement of tattoos and the development of malignant melanoma remains unclear. Our case emphasizes the diagnostic problems of pigmented lesions within tattoos. For safety reasons, tattoos should never be placed on pigmented lesions; if they are, the tattoos should not undergo laser treatment. We suggest an excision before starting laser tattoo removal. Dermoscopic assessments on a regular basis during the period of tattoo removal are recommended. JAMA Dermatol. 2013;149(9):1087−1089. doi:10.1001/jamadermatol.2013.4901 Published online July 31, 2013
The number of decorative tattoos has been increasing, as has the demand for their removal by laser devices. Traumatic events, such as UV and ionizing radiation, mechanical trauma, persistent inflammatory reactions, and burning, have been discussed as cofactors for neoplasm.1,2 Only 16 cases in the English literature document malignant melanoma developing in tattoos.3−5 We herein describe a malignant melanoma that developed on a nevus within a tattoo that had undergone removal by laser.
Report of a Case A white man aged 29 years presented to our clinic for the
first time in 2001 to have his decorative tattoos removed by laser. The large
multicolored tattoos on both arms and his chest had been applied approximately
10 years earlier (Figure 1). After detailed informed consent, we started tattoo
removal in March of 2002 using
 Owing to
the extreme size of the tattoo, only partial treatment could be applied during
each session. Because of a loss of response after 43 sessions, we started using
Owing to
the extreme size of the tattoo, only partial treatment could be applied during
each session. Because of a loss of response after 43 sessions, we started using
 Discussion Before laser tattoo removal, skin should be examined as
thoroughly as possible for hidden pigmented lesions. In cases of nonadherence
to medical advice (as discussed herein), laser treatment should be withheld
until the recommended excision has taken place. Suspicious nevi can be covered
by tattoos, and assessing the nevi is extremely difficult at the clinical and
dermoscopic levels.6 Tattooing also causes difficulties in assessing a sentinel
lymph node biopsy specimen because the pigment can mimic metastatic disease and
thus provide a challenge for surgeons and pathologists.7 We
recommend dermoscopic assessments on a regular basis while a tattoo is
undergoing removal by laser. For this reason, laser removal of tattoos should
be performed by dermatologists and not by nonprofessionals.8
Discussion Before laser tattoo removal, skin should be examined as
thoroughly as possible for hidden pigmented lesions. In cases of nonadherence
to medical advice (as discussed herein), laser treatment should be withheld
until the recommended excision has taken place. Suspicious nevi can be covered
by tattoos, and assessing the nevi is extremely difficult at the clinical and
dermoscopic levels.6 Tattooing also causes difficulties in assessing a sentinel
lymph node biopsy specimen because the pigment can mimic metastatic disease and
thus provide a challenge for surgeons and pathologists.7 We
recommend dermoscopic assessments on a regular basis while a tattoo is
undergoing removal by laser. For this reason, laser removal of tattoos should
be performed by dermatologists and not by nonprofessionals.8
Pigmented lesions should not be treated by laser because of forensic
considerations and to prevent potential laserinduced changes. In 2004, Kerl et
al9 published a tale of caution concerning laser therapy and melanocytic nevi
and emphasized that, for most melanocytic lesions, laser therapy is not
appropriate.9 No scientific evidence suggests that laser treatment
converts benign nevi into melanoma, and we will never know if the nevus in our
case would have progressed the same way with or without laser treatment. In the
course
Kopera et al10 already described the pitfalls of treating
melanocytic lesions by laser:
They found that treating pigmented lesions with a laser delays the diagnosis of melanoma and thus prevents the timely beginning of the necessary therapy. The authors suggest that laser treatment of melanocytic nevi is often based on a clinical or histological misdiagnosis and that more unreported cases exist. They also raise the question of the possibility of melanoma induction by laser. Lee and Busam15 emphasize the importance of dermoscopy and, if necessary, performing appropriate biopsies before laser treatment. With these aspects in mind, we would make a different decision in the future and exclude pigmented lesions within tattoos from laser treatment in general. In the present case, we want to emphasize the diagnostic problems of pigmented lesions within tattoos and the danger
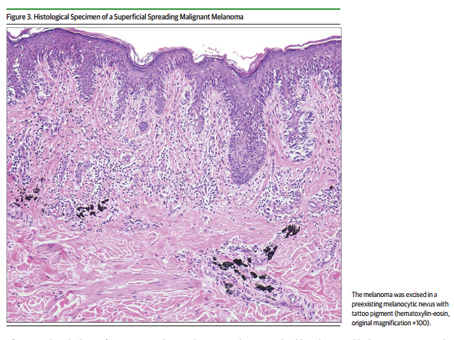 ARTICLE INFORMATION Accepted for Publication: April 4, 2013.
Published Online: July 31, 2013. doi:10.1001/jamadermatol.2013.4901. Author
Contributions: All authors had full access to all the data in the study and
take responsibility for the integrity of the data and the accuracy of the data
analysis. Study concept and design: All authors. Acquisition of data: Pohl.
Analysis and interpretation of data: Raulin. Drafting of the manuscript: Pohl.
Critical revision of the manuscript for important intellectual content: All
authors. Statistical analysis: Raulin. Administrative, technical, or material
support: All authors. Study supervision: Raulin. Conflict of Interest
Disclosures: None reported. Additional Contributions: Markus Hantschke, MD,
Dermatopathologie Friedrichshafen, Germany, provided the image used in Figure
3.
ARTICLE INFORMATION Accepted for Publication: April 4, 2013.
Published Online: July 31, 2013. doi:10.1001/jamadermatol.2013.4901. Author
Contributions: All authors had full access to all the data in the study and
take responsibility for the integrity of the data and the accuracy of the data
analysis. Study concept and design: All authors. Acquisition of data: Pohl.
Analysis and interpretation of data: Raulin. Drafting of the manuscript: Pohl.
Critical revision of the manuscript for important intellectual content: All
authors. Statistical analysis: Raulin. Administrative, technical, or material
support: All authors. Study supervision: Raulin. Conflict of Interest
Disclosures: None reported. Additional Contributions: Markus Hantschke, MD,
Dermatopathologie Friedrichshafen, Germany, provided the image used in Figure
3.
REFERENCES
-
Khan IU, Moiemen NS, Firth J, Frame JD. Malignant melanoma disguised by a tattoo [case report]. Br J Plast Surg. 1999;52(7):598.
-
Kluger N, Phan A, Debarbieux S, Balme B, Thomas L. Skin cancers arising in tattoos: coincidental or not? Dermatology. 2008;217(3):219−221.
-
Paradisi A, Capizzi R, De Simone C, Fossati B, Proietti I, Amerio PL. Malignant melanoma in a tattoo: case report and review of the literature. Melanoma Res. 2006;16(4):375−376.
-
Varga E, Korom I, Varga J, Kohán J, Kemény L, Oláh J. Melanoma and melanocytic nevi in decorative tattoos: three case reports.J Cutan Pathol. 2011;38(12):994−998.
-
Kluger N, Koljonen V. Tattoos, inks, and cancer. Lancet Oncol. 2012;13(4):e161−e168.
-
Gall N, Bröcker EB, Becker JC. Particularities in managing melanoma patients with tattoos: case report and review of the literature.J Dtsch Dermatol Ges. 2007;5(12):1120−1121.
-
Singh RS, Hafeez Diwan A, Prieto VG. Potential diagnostic pitfalls in melanoma arising in a cutaneous tattoo. Histopathology. 2007;51(2):283−285.
-
Karsai S, Krieger G, Raulin C. Tattoo removal
by non-professionals: medical and forensic considerations.J Eur Acad Dermatol Venereol. 2010;24(7):756−762. -
Kerl H, Raulin C, Landthaler M. Controversy in dermatology: laser therapy and melanocytic nevi [in German].J Dtsch Dermatol Ges. 2004;2(8): 681−683.
-
Kopera D, Hohenleutner U, Stolz W, Landthaler M. Ex vivo
quality-switched ruby laser irradiation of cutaneous melanocytic lesions: persistenceof S-100–, HMB-45– and Masson-positive cells. Dermatology. 1997;194(4):344−350. -
Kaskel P, Kind P, Sander S, Peter RU, Krähn G. Trauma and melanoma formation: a true association? Br J Dermatol. 2000;143(4):749−753.
-
12. Lehner K, Santarelli F, Vasold R, König B, Landthaler M, Bäumler W. Black tattoo inks are a source of problematic substances such as dibutyl phthalate. Contact Dermatitis. 2011;65(4):231−238.
-
Gottschaller C, Hohenleutner U, Landthaler M. Metastasis of a malignant melanoma 2 years after carbon dioxide laser treatment of a pigmented lesion: case report and review of the literature. Acta Derm Venereol. 2006;86(1):44−47.
-
Zipser MC, Mangana J, Oberholzer PA, French LE, Dummer R. Melanoma after laser therapy of pigmented lesions: circumstances and outcome. Eur J Dermatol. 2010;20(3):334−338. 15. Lee EH, Busam KJ. Desmoplastic melanoma presenting after laser treatment: a case report and tale of caution. Dermatol Surg. 2011;37(11):1689−1692.
.jpg)